SENIORS: This Sleeping Behavior May Raise Your Stroke Risk
As we age, many of us become more aware of lifestyle habits that affect our heart, brain, and overall vascular health. Sleep is one of those often-overlooked factors. Emerging research suggests that how you sleep — not just how long — could influence your risk of stroke, especially in later years.
In this article, we look at the evidence, clarify the risks, and offer tips on safer sleep postures for seniors.
Why Sleep Matters for Stroke Risk
Sleep is not just “rest.” It’s a critical period for your body to regulate blood pressure, repair blood vessels, clear metabolic waste, and maintain healthy brain function. Poor sleep — including fragmented sleep, abnormal sleep durations, or breathing problems like obstructive sleep apnea — has been linked with higher risks of stroke and other cardiovascular events. (PubMed Central)
Key findings from research:
- In a prospective meta-analysis, long sleep durations (more than ~8–9 hours) were associated with a significantly higher risk of stroke incidence and mortality. (SpringerLink)
- Short sleep (≤ 5–6 hours) is also associated with increased stroke risk, though the evidence is more mixed. (SpringerLink)
- Sleep disruptions — frequent awakenings or fragmented sleep — are tied to signs of small vessel damage in the brain and vascular injury. (smhvenice.com)
- In older adults, severe obstructive sleep apnea (OSA) is a strong, independent risk factor for ischemic stroke. (AHA Journals)
All of this suggests that not only the quantity but also the quality, continuity, and posture of sleep are essential.
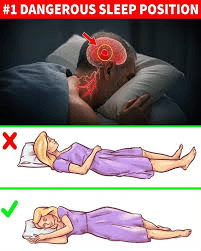
Which Sleeping Position Raises the Most Concern?
While the research is still evolving, one posture that draws attention is lying flat on your back (supine), especially when combined with other risk factors like breathing disorders.
Supine (Back) Position and Stroke Risk
- Worsening sleep apnea: Sleeping on your back tends to worsen obstructive sleep apnea (OSA). When you lie supine, your airway is more likely to collapse, increasing apnea episodes, intermittent drops in oxygen levels, and surges in blood pressure — all risk factors tied to stroke. (PubMed Central)
- Positional influence after stroke: In studies of stroke patients, many tend to spend the majority of their sleep time lying on their backs (supine) in the acute phase. This may exacerbate apnea burden and impact recovery. (PubMed Central)
- Mechanical risks with neck rotation: In rare case reports, sleeping in a prone position with extreme neck rotation has been implicated in compressing vertebral arteries, causing strokes in the posterior circulation (so-called “bow-hunter’s stroke”). (ScienceDirect)
While these findings don’t prove that supine sleep causes strokes directly, they point to mechanisms and associations worth considering — especially for seniors with other vascular risk factors.
Balancing the Evidence: What the Research Doesn’t Show
It’s important to keep perspective:
- Most studies are observational, meaning they show associations — not definitive cause and effect.
- Many findings focus more on sleep duration, fragmentation, or breathing disorders than on posture alone. (PubMed Central)
- What’s “risky” for one person may not be for another, depending on age, health status, neck/spine anatomy, and existing vascular disease.
- Some older adults simply find certain positions more comfortable (or only tolerable) due to other health issues (arthritis, back pain, respiratory problems, etc.).
So rather than prescribing a single “perfect” position, the goal is to adopt safer habits suited to your body and risks.
Safer Sleep Tips for Seniors — Protecting Brain & Blood Flow
Here are practical, evidence-informed strategies seniors can adopt to support healthier sleep and reduce stroke risk:
- Favor side-sleeping (lateral) when possible
- Sleeping on your side reduces airway collapse compared to supine.
- The “left lateral” position may even support better venous drainage from the brain.
- Elevate the upper body slightly
- Use pillows or an adjustable bed to raise your head and torso (e.g. 30° incline).
- This can lessen breathing obstruction, reduce snoring, and improve circulation.
- Avoid extreme neck rotation or hyperextension
- Don’t twist your neck sharply to one side for extended periods.
- Use pillows that maintain neutral alignment.
- Treat sleep apnea if present
- If you snore heavily, wake gasping, or feel tired during the day, ask your doctor about sleep studies and CPAP therapy. Severe OSA significantly increases stroke risk in older adults. (AHA Journals)
- Limit excessively long sleep or naps
- Aim for a regular sleep schedule of ~7–8 hours per night (for many older adults).
- Limit longer naps (>90 minutes). Disrupted or excessive sleeping is correlated with vascular risk. (aan.com)
- Promote continuity & reduce sleep fragmentation
- Good sleep hygiene (consistent bedtime, avoiding late caffeine, comfortable bedroom, limiting noise/light) helps reduce awakenings that stress blood vessels.
- Fragmented sleep has been associated with vascular damage in older adults. (smhvenice.com)
- Stay physically active & control cardiovascular risk factors
- Exercise, blood pressure control, cholesterol management, diabetes control, and quitting smoking all reduce stroke risk and also help improve sleep quality.
Conclusion
While there is no single “bad” sleeping position proven to directly cause stroke, the supine (flat-on-back) posture raises particular concerns in seniors, especially when sleep apnea or vascular vulnerabilities are present. For many older adults, shifting toward side-sleeping, elevating the head, and managing breathing disorders may offer a safer approach.
If you’re over 60 (or caring for someone who is), this is one more reason to take sleep seriously — not just for rest, but for protecting your brain and circulation.
⚠️ Disclaimer: This information is for educational purposes and not medical advice. Always consult your physician before making significant changes to sleep posture or seeking sleep disorder treatment.